Building a mobile app in 2026 is no longer about chasing the lowest quote. It’s about investing in the right architecture, compliance, and scalability from day one.
As a trusted mobile application development company, Taction Software helps startups, healthcare organizations, and enterprises across the U.S. understand how much it really costs to build an app—and how to avoid budget overruns.
Check Now: Click Here
How Much Does It Cost to Build an App?
In the U.S., the average app development cost falls into these ranges:
| App Type | Cost Range |
|---|---|
| Simple MVP / Utility App | $25,000 – $60,000 |
| Startup MVP | $60,000 – $120,000 |
| Mid-Complexity Business App | $120,000 – $200,000 |
| Healthcare / Fintech App | $150,000 – $350,000+ |
| Enterprise App Platform | $250,000 – $500,000+ |
If you’re comparing vendors that offer custom mobile app development services, these numbers reflect real production-ready builds—not templates.
Why App Development Cost Varies So Much
Two apps can both be labeled “MVPs” and still differ by over $150,000. The difference usually comes down to features, integrations, and compliance requirements.
For example, a basic booking app costs far less than a HIPAA-compliant scheduling system like those described in our guide on
appointment scheduling app development for healthcare providers.
Key cost drivers include:
Number of user roles (admin, user, provider)
Platform choice (iOS, Android, cross-platform)
Backend logic and APIs
Security and regulatory needs
Team experience and delivery model
Transform Your App Development Process with Taction
App Development Cost Breakdown by Phase
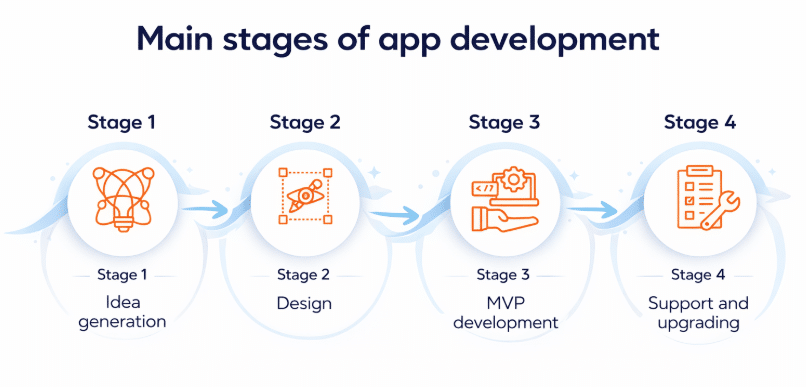
Discovery & Product Strategy
Cost: $4,000 – $8,000
Discovery defines scope, architecture, and budget expectations. Skipping this step is the most common reason apps exceed budget—especially in custom healthcare app development, where compliance planning is critical.
Learn more about early-stage healthcare planning in
custom healthcare app development for small clinics.
UI/UX Design & Prototyping
Cost: $12,000 – $30,000
Design includes wireframes, clickable prototypes, and usability testing. This phase is especially important for businesses working with a healthcare app development company, where user experience directly impacts adoption.
Examples of region-specific healthcare solutions:
App Development (Core Build)
Cost: $35,000 – $120,000+
Share of total cost: 50–70%
This phase includes frontend, backend, APIs, admin panels, and integrations. Many businesses reduce costs by choosing cross platform mobile application development, which we implement across projects like
custom software development in the USA and
custom software development in California.
QA Testing & Security Validation
Cost: $8,000 – $20,000
QA ensures performance, security, and compatibility. This is mandatory for apps built under custom healthcare compliance solutions, where data protection is non-negotiable.
Explore our approach to compliance-driven builds here:
custom healthcare compliance solutions
Deployment & Launch
Cost: $2,000 – $4,000
Includes App Store submission, Play Store approval, CI/CD pipelines, and production setup.
App Maintenance & Support
Annual Cost: ~20–25% of development cost
Maintenance covers updates, bug fixes, security patches, and cloud infrastructure.
App Development Cost by Complexity
| App Complexity | Cost Range | Examples |
|---|---|---|
| Simple | $30k – $40k | Internal tools |
| Medium | $50k – $90k | Booking systems |
| Large | $80k – $150k | Marketplaces |
| Complex | $160k – $300k | Healthcare platforms |
| Enterprise | $250k+ | EHR-integrated systems |
Healthcare platforms—such as those built through our
doctor appointment app development company—typically fall into the higher tiers.
Feature-Level App Development Cost
Basic Features
User authentication: $1k–$4k
User profiles: $1k–$3k
Push notifications: $1.5k–$3k
Analytics setup: $1k–$2k
Advanced Features
| Feature | Cost |
|---|---|
| Payment gateway | $4k – $6k |
| AI / Machine Learning | $20k – $50k+ |
| Geolocation | $4k – $10k |
| IoT / BLE integration | $9k+ |
| Accessibility (ADA/WCAG) | $15k – $25k |
Advanced features should only be added when they support clear business outcomes.
App Development Cost by Industry
| Industry | Cost Range |
|---|---|
| Healthcare & Telemedicine | $150k – $350k+ |
| Fintech | $150k – $320k+ |
| eCommerce | $100k – $180k |
| On-Demand Apps | $120k – $200k |
| SaaS Platforms | $80k – $180k |
Healthcare apps often require more investment due to compliance and integrations, similar to solutions delivered by our healthcare app development company in Dallas and Austin.
Final Answer: How Much Should You Budget in 2026?
For most U.S. businesses:
$60k–$120k → Revenue-ready MVP
$120k–$250k+ → Scalable, compliant product
Underestimating app development cost usually leads to rewrites, delays, and lost revenue.
Build Your App with Taction Software
Taction Software is a proven mobile app development firm delivering:
Custom mobile and web applications
HIPAA-compliant healthcare software
Enterprise and SaaS platforms
AI-enabled and integration-heavy systems
If you want a transparent, realistic app development cost estimate, our team can help.
Ready to Build Your Mobile App with Agile Excellence?
Clinical Workflows and Care Delivery Models
Effective RPM requires redesigned clinical processes:
Enrollment and Onboarding
Patient Identification and Selection: Successful programs implement clinical criteria defining appropriate candidates, shared decision-making with patients about participation, informed consent addressing monitoring scope and expectations, technology assessment ensuring patient capability, and enrollment tracking managing pipeline.
Device Setup and Training: Structured onboarding includes device delivery and distribution logistics, patient training on device usage, troubleshooting common issues, initial data transmission verification, and follow-up confirming successful adoption.
Baseline Assessment: Clinical establishment of baseline vital signs and norms, current medication reconciliation, treatment goals and targets, care plan documentation, and patient education about condition and monitoring sets foundation for success.
Daily Monitoring Operations
Care Team Structures: Effective monitoring requires defined team roles including RNs or care managers reviewing daily data, physicians supervising and making clinical decisions, medical assistants providing technical support, care coordinators addressing social barriers, and administrative staff managing enrollment and billing.
Data Review Protocols: Efficient workflows include scheduled review times for routine monitoring, real-time alert response for urgent issues, prioritized patient lists focusing attention, documentation templates streamlining notes, and escalation pathways to physicians.
Patient Outreach and Intervention: Proactive communication delivers scheduled check-in calls or messages, response to concerning trends, medication or lifestyle coaching, barrier identification and problem-solving, and encouragement and motivation.
Clinical Decision-Making: Evidence-based protocols guide medication titration algorithms, hospitalization criteria, specialist referral triggers, visit scheduling decisions, and monitoring frequency adjustments.
Integration with Other Care Modalities
Telehealth Visit Integration: Monitoring data informs video consultation preparation, shared screen review during visits, longitudinal trend discussion, collaborative goal adjustment, and post-visit documentation.
Organizations should ensure seamless connection between RPM and telemedicine app development in USA platforms creating unified patient experiences.
In-Person Care Coordination: Clinic visit preparation using monitoring data, emergency department integration for acute events, hospital discharge transition with monitoring continuation, specialty care coordination, and home health collaboration optimize outcomes.
Care Management Programs: RPM enhances chronic care management (CCM), transitional care management (TCM), principal care management (PCM), behavioral health integration, and medication therapy management creating comprehensive care coordination.
Reimbursement and Financial Sustainability
RPM programs require sound financial models:
Medicare RPM Reimbursement
CPT Code Structure: CPT 99453 ($19) covers initial setup and patient education; CPT 99454 ($65/month) covers device supply and daily monitoring data transmission; CPT 99457 ($51 for first 20 minutes) covers interactive communication and care management; CPT 99458 ($40) covers each additional 20 minutes beyond initial; CPT 99091 ($57) covers collection and interpretation of physiological data.
Billing Requirements: Documentation requirements include physician order for remote monitoring, patient consent documented, 16 days of data transmission per month minimum, 20 minutes of interactive communication monthly, medical necessity justification, and time tracking for care management activities.
Reimbursement Optimization: Maximizing revenue requires accurate time tracking and documentation, appropriate code selection, patient engagement ensuring transmission requirements, comprehensive care management justifying time, denial management and appeals, and regular billing audit and compliance.
Commercial Payer Strategies
Contract Negotiation: Payer engagement addresses telehealth parity advocating for RPM coverage, medical policy development securing coverage decisions, reimbursement rate negotiation, prior authorization requirements, and program design alignment with payer priorities.
Value-Based Arrangements: Alternative payment models include per-member-per-month (PMPM) payments, shared savings based on utilization reduction, bundled payment inclusion, quality bonus opportunities, and pay-for-performance metrics.
Program Cost Management
Technology Costs: Financial planning includes platform licensing or development, device acquisition ($30-$500 per patient), cellular connectivity fees ($5-$15/month per device), infrastructure and hosting, and maintenance and support.
Operational Costs: Staffing requirements for care managers and nurses, physician supervision time, administrative support, training and education, and patient acquisition and marketing drive ongoing expenses.
Economies of Scale: Larger programs achieve lower per-patient device costs through bulk purchasing, shared care team infrastructure, technology cost spreading, and administrative efficiency.
Return on Investment
Revenue Generation: Direct RPM reimbursement, improved chronic care management billing, reduced gaps in care billing, improved quality bonuses, and shared savings from reduced utilization contribute returns.
Cost Savings: Hospital readmission reduction (preventing $10,000-$30,000 per readmission), emergency department diversion ($500-$2,000 per avoided visit), clinic visit efficiency improvements, medication optimization reducing waste, and complication prevention generate savings.
ROI Timeline: Typical programs achieve break-even at 12-18 months with 200-300 enrolled patients, positive returns accelerating at scale, 3-year ROI of 150-300% for successful programs, and higher returns in value-based contracts.
Organizations should work with HIPAA-compliant software development in USA partners understanding healthcare reimbursement landscapes ensuring platforms capture all billable services and support financial sustainability.
Regulatory Compliance and Quality Assurance
RPM platforms navigate complex regulatory environments:
FDA Medical Device Considerations
Software as a Medical Device (SaMD): FDA regulates software that diagnoses or treats conditions, analyzes physiological data for clinical decisions, or controls medical devices, while exempting administrative functions, electronic health records, general wellness applications, and patient engagement tools without diagnostic claims.
Risk-Based Classification: Class I (low risk) general controls, Class II (moderate risk) requiring 510(k) clearance, and Class III (high risk) requiring PMA approval determine regulatory pathway. Most RPM platforms constitute Class II devices requiring FDA clearance.
Quality System Regulations: Medical device manufacturers must implement design controls documenting development and validation, risk management per ISO 14971, design verification and validation, document and change control, and post-market surveillance.
Clinical Evaluation: FDA expects clinical validation demonstrating intended use fulfillment, usability testing with representative users, performance validation across diverse populations, and outcome measurement showing clinical benefit.
HIPAA and Data Privacy
RPM platforms handling protected health information require comprehensive HIPAA-compliant app development in USA including administrative safeguards (security management, workforce training, contingency planning), physical safeguards (device and media controls, workstation security), technical safeguards (access controls, encryption, audit logs, authentication), breach notification procedures, and business associate agreements.
State Privacy Laws: California Consumer Privacy Act (CCPA) and other state laws create additional requirements for consumer rights, data minimization, transparency obligations, and opt-out mechanisms.
Clinical Validation and Evidence
Outcome Measurement: Programs should track clinical quality metrics (disease-specific outcomes), patient-reported outcomes and satisfaction, healthcare utilization (hospitalizations, ED visits), care team efficiency and productivity, and financial performance and ROI.
Quality Improvement: Continuous monitoring includes patient safety event tracking, device malfunction reporting, clinical protocol adherence, alert response time measurement, and regular program evaluation.
Evidence Generation: Peer-reviewed publication, registry participation, quality measure reporting, and patient testimonials build credibility and support payer contracting.
Implementation Best Practices
Successful RPM deployment requires systematic approaches:
Pilot Program Strategy
Focused Launch: Begin with single high-value condition (heart failure, diabetes, hypertension), limited patient population (50-100 patients), experienced enthusiastic providers, dedicated implementation support, and intensive monitoring and adjustment.
Learning Objectives: Validate clinical workflows and protocols, test technology reliability and usability, identify training and support needs, establish baseline metrics, and build organizational capabilities.
Expansion Planning: Apply lessons learned from pilot, standardize successful processes, scale infrastructure and resources, broaden conditions and populations, and establish ongoing governance.
Patient Selection and Engagement
Enrollment Criteria: Target patients with high-risk conditions, recent hospitalizations, sub-optimal disease control, technology capability and willingness, and adequate caregiver support when needed.
Engagement Strategies: Motivational interviewing and shared decision-making, clear communication about program expectations and benefits, ongoing education and support, recognition and rewards for adherence, and family/caregiver involvement drive participation.
Addressing Barriers: Technology training and support, device provision and financial assistance, language and literacy accommodation, care coordination for social needs, and flexible program design supporting diverse populations enable success.
Care Team Training and Support
Clinical Training: Disease-specific monitoring protocols, device operation and troubleshooting, data interpretation and clinical decision-making, documentation and billing requirements, and patient communication and coaching skills support effective monitoring.
Operational Training: Platform navigation and workflows, alert management and prioritization, time tracking and documentation, care coordination processes, and quality improvement participation enable efficient operations.
Ongoing Support: Regular case conferences and peer learning, performance feedback and coaching, protocol updates and best practice sharing, technology enhancement training, and burnout prevention and wellness attention maintain capabilities.
Technology Partner Selection
Organizations should evaluate RPM vendors on device ecosystem breadth and integration quality, platform scalability and reliability, clinical workflow optimization, analytics and intelligence capabilities, EHR and system integration, compliance and security rigor, implementation and support services, financial model and cost structure, evidence and customer references, and long-term viability and innovation roadmap.
Experienced partners like Taction Software with extensive healthcare technology experience (785+ healthcare clients over 20+ years) and proven mHealth apps development bring specialized knowledge ensuring successful implementation.
Case Study: Comprehensive RPM Program Implementation
A regional health system serving 500,000 patients across urban and rural communities launched comprehensive remote monitoring addressing high readmission rates, sub-optimal chronic disease control, and value-based contract performance requirements.
Clinical Objectives: Reduce 30-day heart failure readmissions by 30%, improve diabetes control (HbA1c<8%) by 20 percentage points, increase hypertension control rates by 15%, enhance patient engagement and satisfaction, and achieve positive program ROI within 18 months.
Program Design: Multi-condition RPM platform supporting heart failure with daily weight, blood pressure, pulse oximetry, and symptom monitoring; diabetes with blood glucose monitoring and CGM integration; hypertension with blood pressure monitoring; COPD with pulse oximetry and symptom tracking; and post-surgical monitoring with vital signs and wound assessment. Care team structure included dedicated RPM nurses reviewing data and conducting outreach, care coordinators addressing barriers, supervising physicians making clinical decisions, and integration with existing care management programs. Technology approach utilized medical-grade cellular-connected devices minimizing patient burden, tablet-based symptom assessment for less tech-savvy patients, smartphone app for younger populations, Taction Software mHealth platform with comprehensive analytics, and Epic EHR integration via FHIR for seamless workflows.
Implementation Phases:
- Phase 1 (Months 1-3): Heart failure pilot with 75 high-risk patients, care team training and workflow development, device distribution and patient training, daily monitoring protocols establishment, and metric tracking validation.
- Phase 2 (Months 4-8): Expansion to 300 heart failure patients, diabetes monitoring addition (200 patients), hypertension program launch (150 patients), care team expansion and training, and analytics dashboard refinement.
- Phase 3 (Months 9-12): COPD and post-surgical monitoring addition, rural clinic integration expanding geographic reach, predictive analytics implementation, patient portal enhancements, and comprehensive outcome evaluation.
Technology Implementation: Taction’s HIPAA-compliant architecture ensured data security across 650+ monitored patients. Real-time alert engine with machine learning prioritization reduced alert fatigue 40%. Predictive analytics identified high-risk patients 7-10 days before events. Comprehensive analytics tracked clinical, operational, and financial metrics. Cellular devices with autonomous transmission achieved 94% daily compliance. Epic integration automated documentation and billing capture.
Clinical Outcomes (12-month evaluation):
- Heart failure 30-day readmissions decreased 38% (exceeding 30% goal)
- Diabetes HbA1c<8% achievement improved 23 percentage points
- Hypertension control increased 18%
- COPD exacerbation hospitalizations decreased 32%
- Post-surgical complication detection improved 40%
- Patient satisfaction 91% (Net Promoter Score +67)
Operational Results:
- 650 patients enrolled across five conditions
- 94% device transmission compliance rate
- 89% patient retention at 12 months
- Care team managing 130 patients per FTE (vs. 60-80 typical)
- Average response time to critical alerts: 28 minutes
- Documentation time reduced 35% through EHR integration
Financial Performance:
- RPM reimbursement: $468,000 annually
- Avoided readmissions: $1,240,000 (124 prevented readmissions)
- Avoided ED visits: $312,000 (156 prevented visits)
- Improved quality bonuses: $185,000
- Total benefit: $2,205,000
- Program costs: $845,000 (technology, devices, staffing, overhead)
- Net benefit: $1,360,000
- ROI: 161% in first full year
Strategic Impact:
- ACO shared savings significantly improved through utilization reduction
- Medicare Advantage quality star ratings increased
- Competitive differentiation for employer contracts
- Provider satisfaction improved through proactive care tools
- Rural access expanded without facility investment
- Platform foundation for future digital health initiatives
This implementation demonstrates RPM potential when approached strategically with appropriate technology, comprehensive clinical workflows, patient engagement focus, care team training, and commitment to continuous improvement based on data.
Conclusion
Remote patient monitoring represents healthcare’s evolution from reactive episodic care to proactive continuous management, leveraging IoT devices, wearable technology, and sophisticated analytics transforming chronic disease care delivery. Evidence consistently demonstrates RPM effectiveness in improving clinical outcomes, reducing hospitalizations and emergency utilization, engaging patients in self-management, and generating positive return on investment.
Success requires comprehensive platforms integrating diverse medical devices and wearables, sophisticated real-time analytics providing actionable clinical intelligence, efficient care team workflows scaling monitoring across large populations, patient engagement strategies driving adherence and participation, sustainable financial models capturing reimbursement while managing costs, and regulatory compliance ensuring patient safety and data protection.
Healthcare organizations should partner with experienced development companies combining healthcare domain expertise with IoT, mobile, and analytics technical capabilities. Companies like Taction Software, with extensive healthcare application experience and proven mHealth solutions development including comprehensive RPM platforms, bring specialized knowledge translating clinical vision into operationally effective, financially sustainable, and clinically valuable remote monitoring programs.
As value-based care models increasingly define healthcare reimbursement and patient expectations continue favoring convenient digital health access, remote patient monitoring will evolve from innovative pilot programs to essential care delivery infrastructure. Organizations investing strategically in sophisticated RPM platforms today position themselves for leadership in healthcare’s increasingly digital, data-driven, and proactive future.
Frequently Asked Questions
The cost to build an app in the USA typically ranges from $60,000 to $250,000+ in 2026. The final price depends on factors such as app complexity, platform choice (iOS, Android, or cross-platform), backend integrations, and compliance requirements. Regulated solutions—such as those built by a healthcare app development company—usually fall toward the higher end due to security and HIPAA requirements.
The healthcare app development cost usually starts at $150,000 and can exceed $350,000+ for enterprise-grade platforms. Costs are higher because healthcare apps often require HIPAA compliance, secure authentication, EHR/FHIR integrations, and extensive QA. You can see real-world examples in our guide on custom healthcare app development for small clinics.
Yes. Cross platform mobile application development is typically 30–50% more cost-effective than building separate native iOS and Android apps. Frameworks like React Native and Flutter allow a shared codebase, faster development, and lower long-term maintenance—making them a popular choice for MVPs and startups working with a custom software development agency.
Most mobile apps take:
3–6 months for a startup MVP
6–12+ months for complex or regulated apps
Apps that include advanced features like payments, AI, or healthcare workflows—such as those offered by a doctor appointment app development company—generally take longer due to additional testing and compliance validation.
The biggest factors that influence mobile app development cost include:
Number of user roles and workflows
Feature complexity and integrations
Platform choice (native vs cross-platform)
Backend architecture and scalability
Security and compliance requirements
For example, apps built under custom healthcare compliance solutions require additional investment to meet regulatory standards.
App maintenance typically costs 20–25% of the original development cost per year. Maintenance includes bug fixes, OS updates, security patches, cloud hosting, and third-party service fees. Apps in healthcare and enterprise environments require ongoing monitoring and compliance updates, increasing long-term costs.
Yes—if done strategically. You can reduce app development cost by:
Validating ideas with prototypes before development
Limiting the MVP to 1–2 core business outcomes
Using cross-platform frameworks
Reusing proven APIs and SDKs
Planning maintenance early
Working with an experienced mobile app development firm helps avoid the “cheap now, rebuild later” trap.
For most businesses, outsourcing to a specialized mobile application development company is more cost-effective than building an in-house team. Outsourcing eliminates recruitment, infrastructure, and long-term staffing costs while providing access to designers, developers, QA engineers, and compliance experts under one roof.
The most accurate estimates come after a structured discovery phase, which defines scope, architecture, and feature priorities. A reliable estimate should always break costs down by design, development, QA, deployment, and maintenance—rather than offering a single flat number.
Quotes under $10,000–$20,000 usually rely on templates, lack scalability, and ignore security, QA, and maintenance. Many businesses end up rebuilding the app later—often at 2–3× the original cost. Investing upfront with a trusted custom mobile app development services provider avoids this risk.